In planning for Honduras we had to consider several uncertainties: how many patients had been preselected, how many patients we would find eligiblefor surgery, how many patients could be done each day, how much help we would find from the hospital, and what kind of equipment and supplies we would find in the operating room. In order to confront any eventuality we decided to carry our own essential tools: anesthetics, trays of instruments, multiple supplies and the entire set of laparoscopic equipment (monitor, insufflator, and camera unit). We ordered duffle bags, stamped them with “UHMLA Medical Supplies” and off we went.
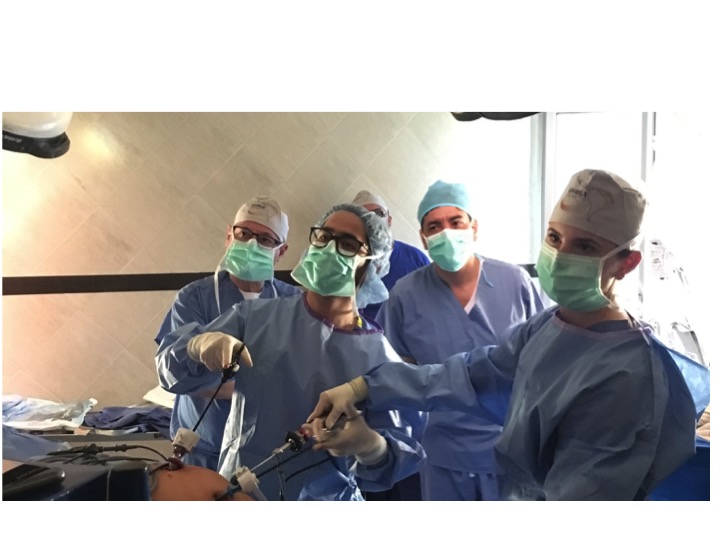
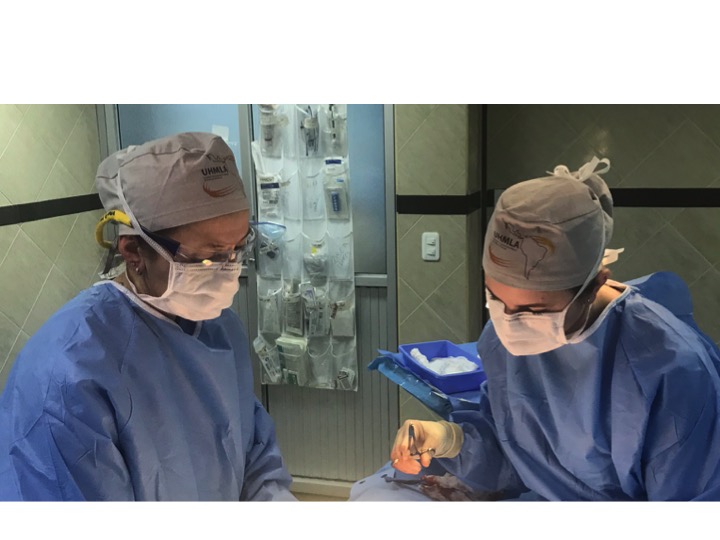
The team was made up by surgical faculty: Rolando Rolandelli, Ted McLean, and Billy Diehl; surgical resident Omar Ahmed, anesthesiologists: Gerry Lefever,, Isaac Spitieri, and Daniel Chung; OR nurses: Imelda Jimenez, and Arlin Fidellaga, PACU nurses: Cyprienne Lacaden and Valentina Salvador, and surgical nurses Monica Grezlak, Ruben Millan, and Carol Santana.
We were anticipating some objections at customs but we crossed without even a single question. Kate from Shoulder to Shoulder was waiting for us in Tegucigalpa with a minibus. We began the process of renting a truck while waiting for Susie Kaye to arrive from Houston. Once Susie arrived and all the luggage was loaded we departed to La Esperanza with a stop in Siguatepeque. In spite the dense fog that hid the huge potholes in the winding road we made to the Apart Hotelwithout incidents.
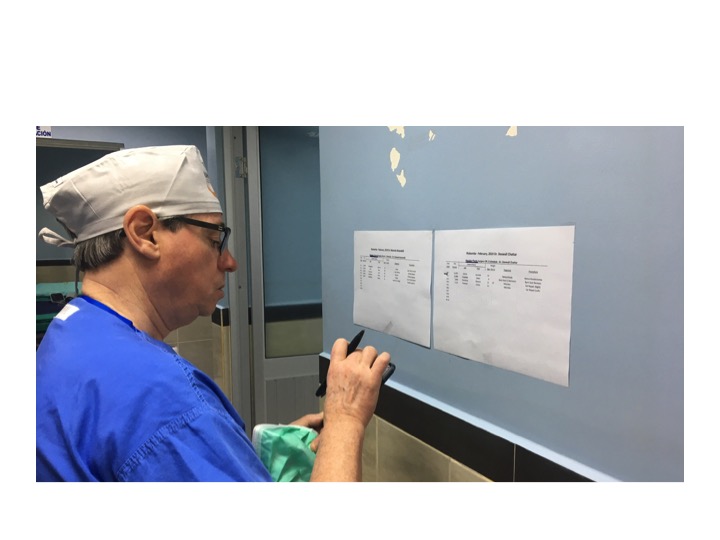
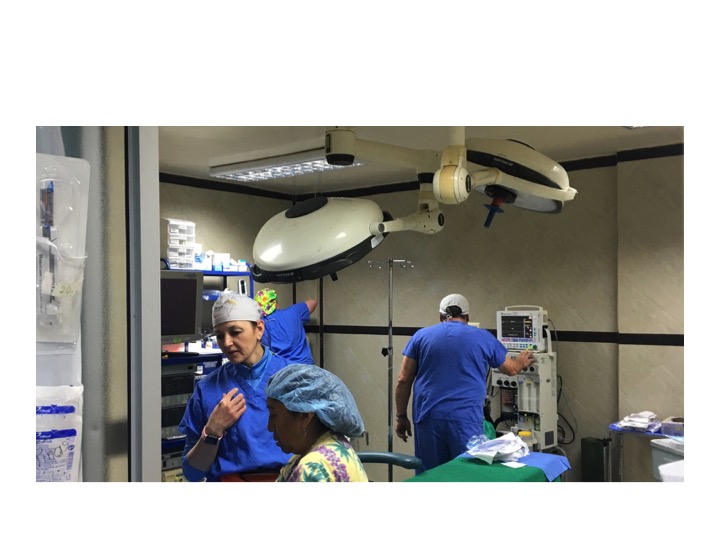
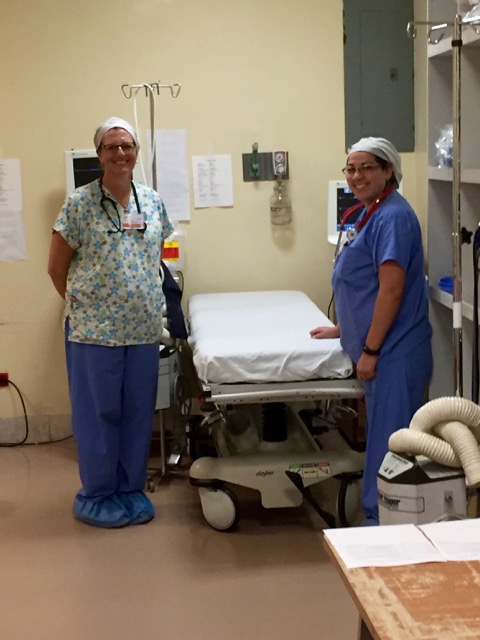
We began early on Sunday at the Hospital Enrique Aguilar Cerrato (HEAC) where we found about 60-70 patients waiting for us and many hospital employees and trainees volunteering time on their day of to help us. At the end of the day we made up the schedule for the entire week in the two operating rooms that were made available to us; one is an active OR which only needed from us the addition of our laparoscopic equipment. The other one had never been used as an operating room, we made it work as such and use a room next to it as a recovery room (Cyprienne was extremely resourceful to make this happen). One problem we faced was that the two ORs were separated by a Labor and Delivery Unit, the busiest any of us had ever seen in our lives. The HEAC provides the obstetric care for women in the immediate region and for all those with high risk pregnancies and/or deliveries in the state of Intibucá of 250,000 people. One number I hear in terms of yearly births was 17,000 which seems high but based on the ones we saw in just 5 days I believe it is totally possible.
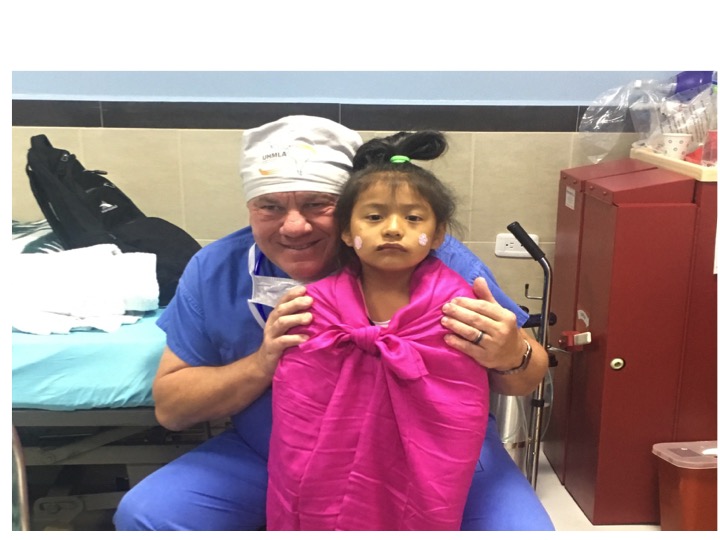
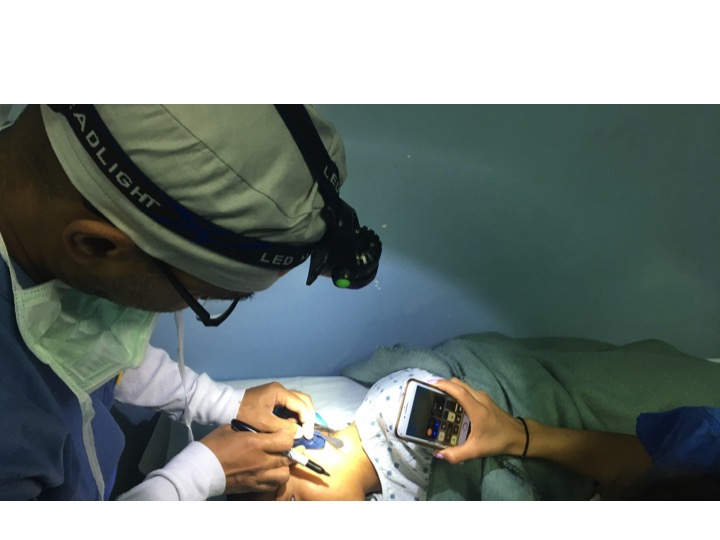
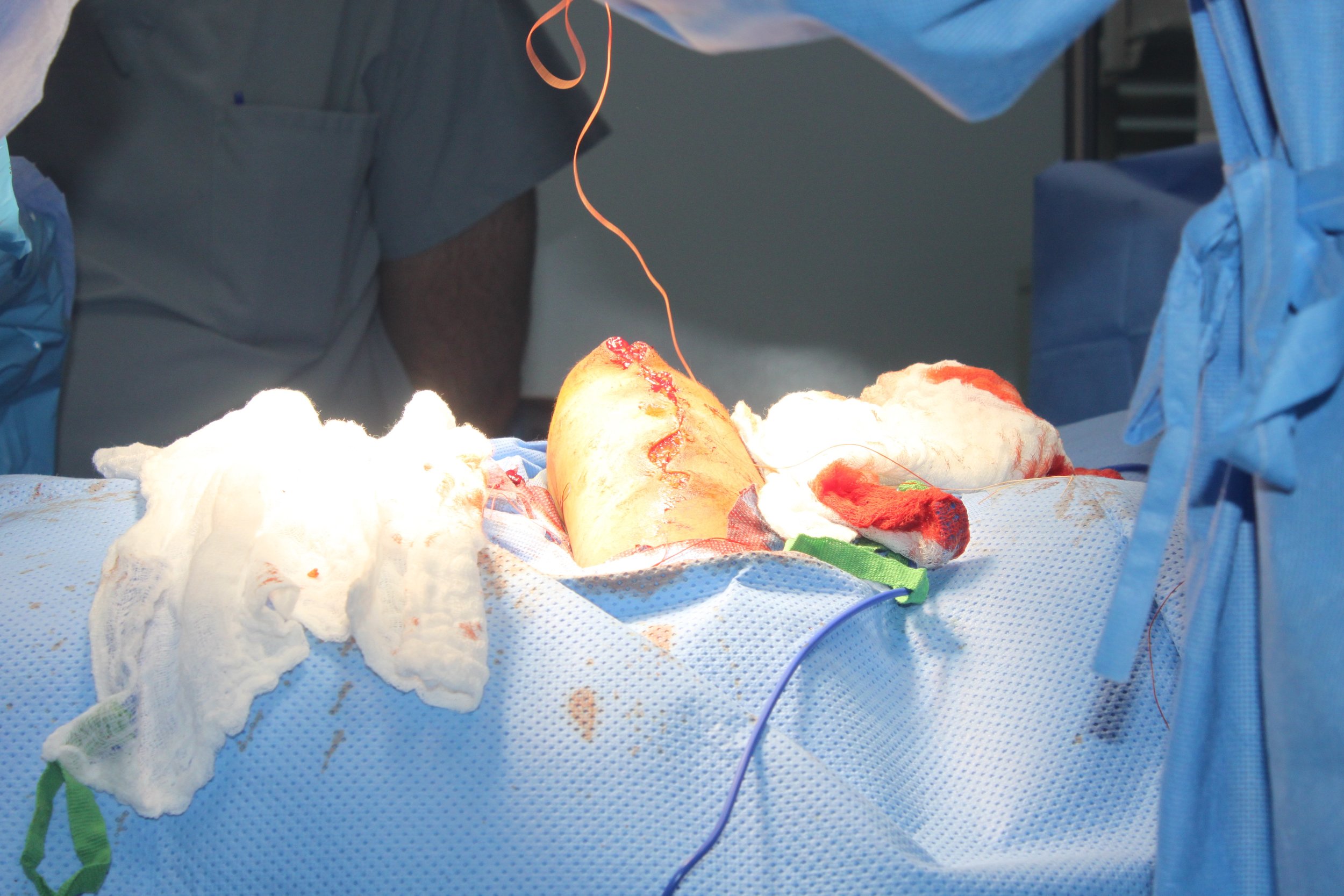
We used the “main” OR for all cholecystectomies, children and any other major cases. In the smaller room we did all the anorectal cases. Hernias fill the gaps in either room. During the weekdays we saw many more patients either in the clinic or the OR. The HEAC normally functions with an anesthesia technician and without intensive care unit. Therefore, patients who are too sick; e.g., any one who may require mechanical ventilation after surgery was transferred out. While we were there we were asked to assist in some of these difficult cases and of course we did what we thought was safe: one elderly woman with acute cholecystitis but we referred out another very malnourished lady with gastric outlet obstruction.
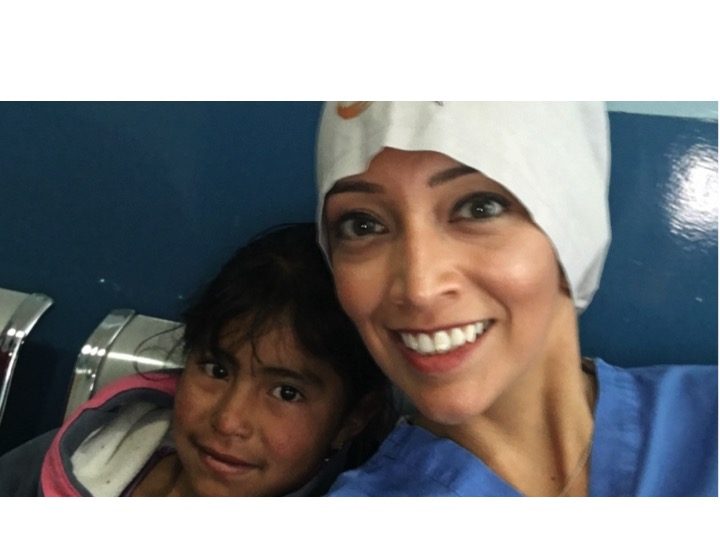
The trip had several highlights for us. First, the collaboration with Shoulder to Shoulder was invaluable; they did an enormous preparatory work and they kept doing it all week long and took responsibility for our patients when we left. Kate who has a Masters in Public Health coordinated everything: patient selection, transport, communication with patients, families and referring physicians, and most important: kept us well fed, hydrated, healthy and happy. We were also fortunate that we had a Board Member of Shoulder to Shoulder Dr. Kaye as part of our Brigade. Susie has more than 15 years of experience in Honduras and with her expertise in Family Practice we were able to sort out issues that exceeded our limited capacity as surgeons. Maggie, who back in New Jersey functions as Dr. Kaye’s administrative assistance came along and offered all of us all kinds of assistance by communicating with patients and families.
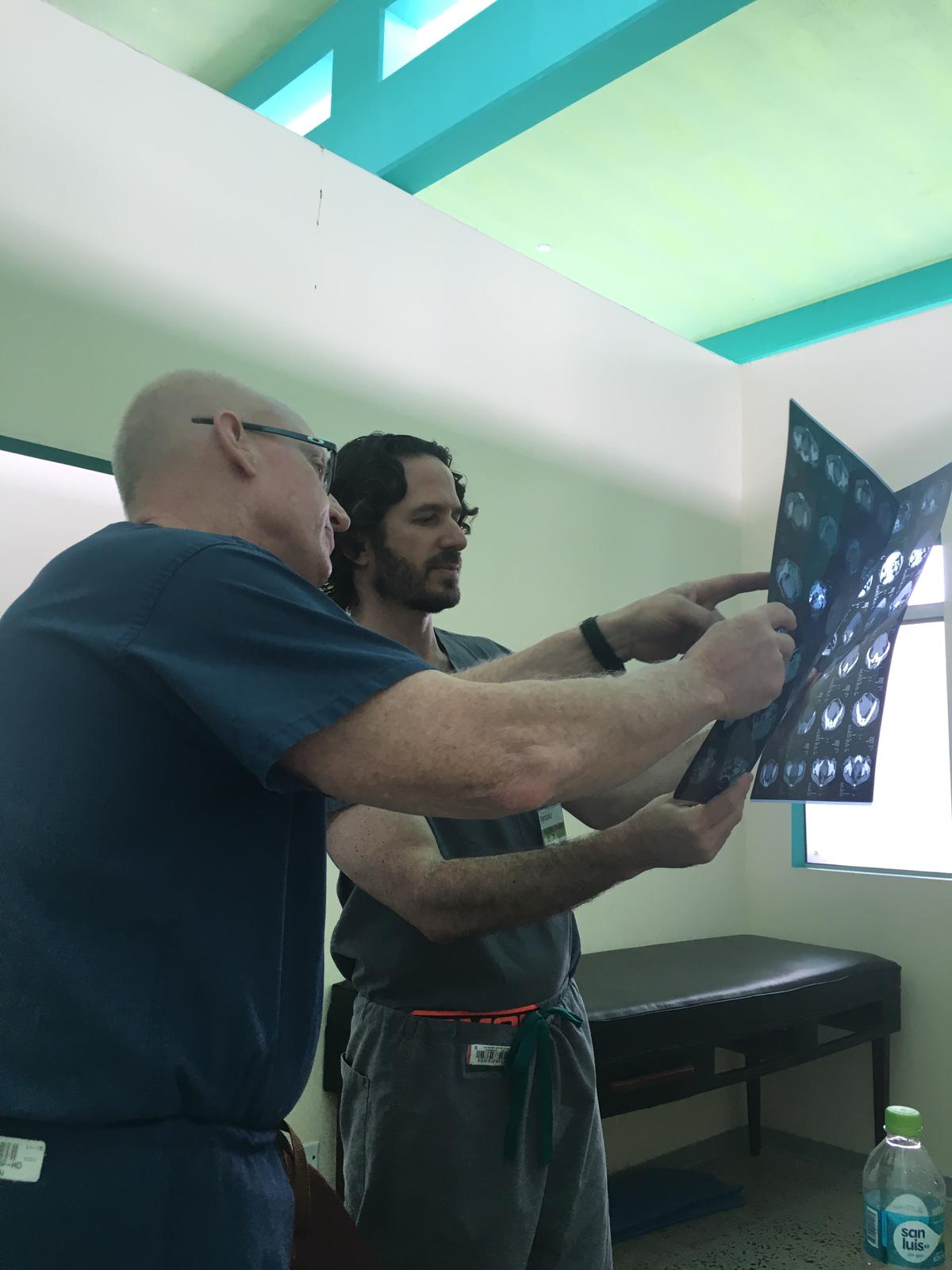
Another highlight of the trip was the opportunity to teach. In Honduras students enter Medical School right after High School, the same way as in many other countries of Europe and South America. Medical School then spans a total of 8 years. All graduates are then required to domandatory rotatory internship in different parts of the country . HEAC takes about 10 of these interns, Doctores Sociales (doctors doing social work). We interacted with many of them, in the clinic doing preoperative assessments and in the wards doing postoperative care. More importantly in the operating room we took them through surgery and we were extremely impressed with their fund of knowledge and surgical skills. Adding medical education of local doctors to the caring for patients in need expends our mission in such a wonderful way and makes these trips so much more rewarding.
At HEAC we counted with the support of the one and only surgeon, Dr. Renee Ratliff, who kept up with his routine responsibilities in addition to making sure we were able to accomplish our mission. He and his wife, the one and only pediatrician Dr. Mene Banegas were very generous and welcomed the entire team of 17 people at their house for a Honduran barbecue. The recently appointed Director of the HEAC , Dr. Benitez, was there as well, and told us that Dr. Ratliff saved the life of his nephew who had sustained a gunshot wound to the torsum that lacerated the inferior vena cava.
We definitely established a bond between UHMLA, Shoulder to Shoulder and HEAC which will keep us going to La Esperanza every year.